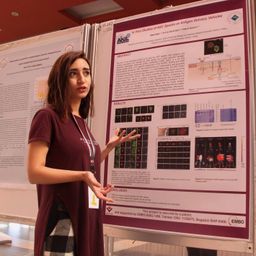
Distinct regulatory T-cell signature of successfully ART-treated HIV-infected individuals with coronary artery disease
Mon statut pour la session
Distinct regulatory T-cell signature of successfully ART-treated HIV-infected individuals with coronary artery disease
Alexis Yero1, Céline Rothan1, Tao Shi1, Omar Farnos1, Carl Chartrand-Lefebvre2,3, Mohamed El-Far2, Petronela Ancuta2,4, Cecilia T. Costiniuk5,6, Christos Tsoukas5,7, Cécile Tremblay2,4, Madeleine Durand2,8, Mohammad-Ali Jenabian1,4,#, for Canadian HIV and Aging Cohort Study.
1
Department of Biological Sciences, CERMO-FC,
Université du Québec à Montréal (UQAM), Montreal,
QC, Canada.
2
CHUM Research Centre, Montreal, QC,
Canada.
3Department of Radiology,
Faculty of Medicine, Université de Montréal, Montreal, QC, Canada.
4
Department of Microbiology, Infectiology
and Immunology, Faculty of
Medicine, Université de Montréal, Montreal, QC, Canada.
5
Research Institute of McGill University Health Centre, Montreal, QC, Canada.
6
Chronic Viral Illness Service and Division of Infectious Diseases, Faculty of Medicine,McGill
University, Montreal, QC, Canada.
7
Division of Clinical Immunology and
Allergy, Faculty of Medicine,McGill
University, Montreal, QC, Canada.
8
Department
of Internal Medicine, Faculty of Medicine, Université de Montréal, Montreal,
QC, Canada.
Background:Chronic inflammation during HIV infection despite antiretroviral therapy (ART) results in accelerated aging and comorbidities, notably atherosclerosis. Total regulatory T-cells (Tregs) and Tregs expressing ectonucleotidases CD39/CD73 are documented to be protective against cardiovascular diseases via their anti-inflammatory functions. We, hereby, assessed Treg subpopulations in ART-treated HIV-infected adults with or without atherosclerosis versus HIV- individuals.
Methods: Blood specimens were obtained from 142 participants including ART-treated HIV-infected adults with (n=43) or without CAD (n=41), as well as HIV-negative individuals with (n=31) or without CAD (n=27). CAD was determined by the presence of atherosclerotic features via computed tomography angiography of the coronary arteries performed on all study participants. Treg subsets frequencies were assessed by flow cytometry.
Results: HIV+CAD+ individuals had the highest total Treg frequencies and increased thymic generation and output of Tregs (Helios/CD31 expression), while athero-protective CD39+/CD73+ Tregs were significantly depleted in this group. Tregs from PLWH had higher expression of CCR6/CXCR3 than uninfected individuals regardless of CAD, while in HIV+CAD+ individuals Tregs expressed the highest levels of CCR4, which limits their maintenance. The lowest levels of CD4 and CD8 T-cell immune activation has been also observed in HIV+CAD+ within study groups.
Conclusions: PLWH under ART with diagnosed CAD are characterized by profound alterations in anti-inflammatory Treg subsets and their migratory signature. The paucity and poor tissue-infiltration potential of anti-inflammatory Treg may represent one of the mechanisms contributing to atherosclerotic plaque formation and progression during chronic HIV infection in the ART era.



Discussion